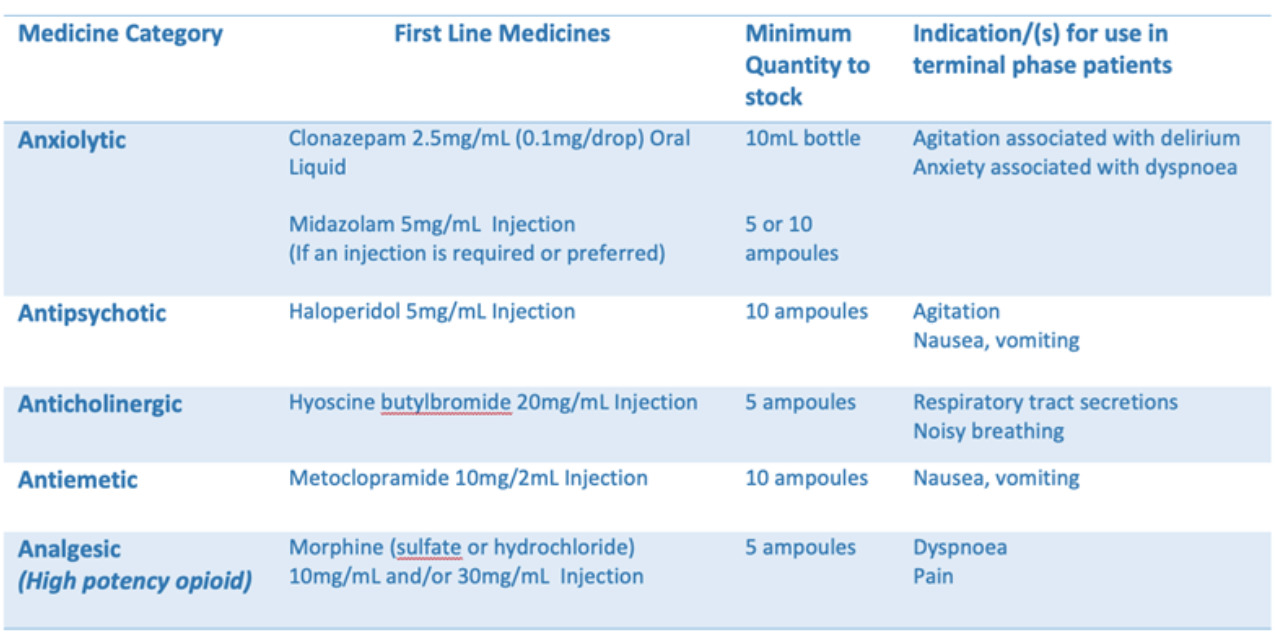
The list includes the medicines endorsed by the Australian and New Zealand Society for Palliative Medicines for use in community-based palliative patients and considered the core palliative care medicine lists published in other states. This list was established for NWMPHN’s region through consultation with local palliative care providers. For this expansion of the project, SEMPHN and EMPHN are using the same list developed in the NWMPHN project to maintain consistency within the metropolitan Melbourne region.
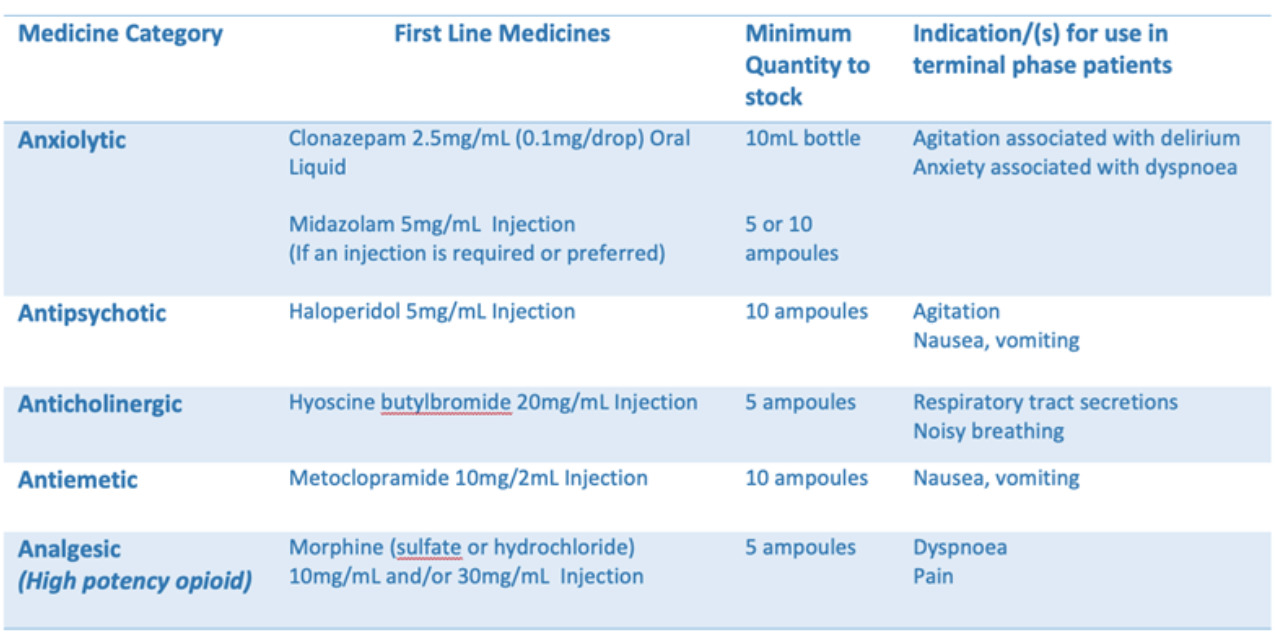
Community pharmacies are encouraged to stock these first-line medicines as this is the recommended list that will be communicated in the region. Additional medicines to the list may be stocked dependent upon local prescribing preferences and/or stock availability.
Note (8 November 2023):
We are aware of some supply issues with metoclopramide injection, including the discontinuation of the PBS-listed Maxolon injection. Alternative brands of metoclopramide have not yet been listed on the PBS. However, as their cost is not prohibitively expensive, our recommendation to prescribers is to continue to prescribe metoclopramide as first line antiemetic medicine. Haloperidol injection (PBS-listed) is also an appropriate alternative therapy for nausea and vomiting in palliative care while these supply issues continue, however it is more sedating.
This list does not restrict which medicines can be prescribed for individual palliative patients as some medicines may not be appropriate in certain circumstances (i.e. metoclopramide/haloperidol is best avoided in Parkinson’s Disease). However, it is one approach which will allow community pharmacies to anticipate medicines most likely to be prescribed allowing prescribers to anticipate medicines most likely to be available for rapid supply in community pharmacies and residential aged care facilities within the metropolitan Melbourne region. We recommend discussing any questions with your local specialist Community Palliative Care service provider.